Read about the features and benefits of the physiologic Freestyle™ bioprosthesis.
Tissue valves and conduits
Freestyle™ aortic root bioprosthesis
<p>The Freestyle™ aortic root bioprosthesis emulates the native aortic valve, designed for hemodynamics and durability.</p>
Features
Durability
Published clinical experience demonstrates impressive long-term performance in many age groups.1 Additional factors that may contribute to durability are:
- Proprietary AOA™ anti-calcification tissue treatment designed to reduce calcification and protect the tissue†
- Physiologic fixation process that reduces the stress applied to the leaflets during fixation
† No clinical data is available which evaluates the long-term impact of the physiologic fixation process or the impact of AOA™ treatment in patients.

AOA™ anti-calcification tissue treatment
Stentless design
By closely mimicking human physiology, the Freestyle™ valve offers excellent hemodynamics and long-term durability.
Excellent clinical performance
- Very low rates of SVD, including a rate of freedom from explant due to SVD‡ of 83% at 15 years1
- Single-digit gradients out to 10 years2
‡ Failure of any component of the bioprosthesis causing stenosis or insufficiency. Excluded is endocarditis and/or thrombosed bioprosthetic valve as cause of dysfunction.
Maximum blood flow
The Freestyle™ valve provides industry-leading hemodynamic performance. Studies have shown the Freestyle™ valve, with its stentless design, has significantly better hemodynamic performance than stented or mechanical aortic surgical valves.3,4 Hemodynamic results with the Freestyle™ valve have shown:
- Larger post-operative effective orifice areas (EOA) than stented or mechanical valves3
- Stable, single-digit gradients and large EOAs at 10 years1

Advanced tissue fixation
Our exclusive physiologic fixation process mitigates biomechanical failures and is engineered for long-term valve durability by:
- Improving preservation of valve structure and leaflet function, allowing it to function like a native valve
- Allowing leaflets to remain soft and flexible, which protects the tissue from cyclic fatigue
Surgical valve replacement risks may include infection, surgical complications, stroke, endocarditis, and death.
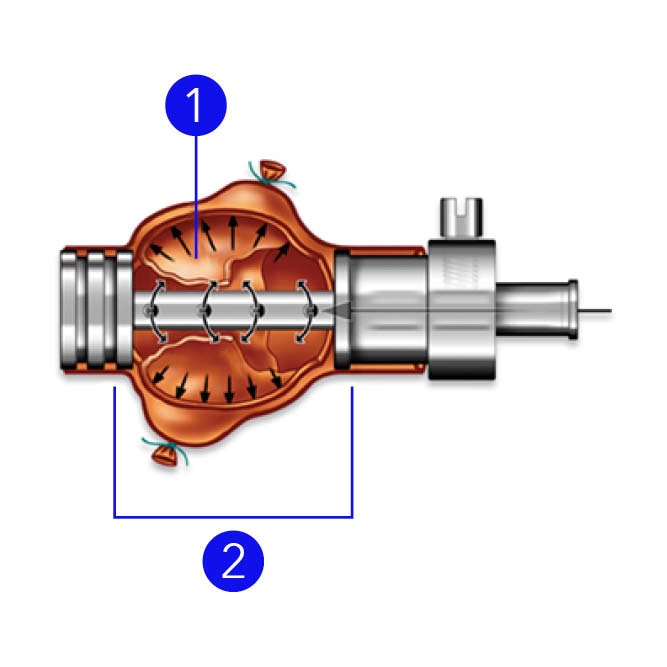
- Leaflets float at net zero pressure
- Roots are pressured at 40 mmHg with glutaraldehyde
Ordering information
Freestyle™ aortic root bioprosthesis
Item number |
Valve size |
Outside diameter |
Profile height |
Inner cloth height (± 0.5 mm) |
(A) |
(B) |
(C) |
||
FR995-19 |
19 |
19.0 |
30 |
3.0 |
FR995-21 |
21 |
21.0 |
32 |
3.0 |
FR995-23 |
23 |
23.0 |
32 |
3.0 |
FR995-25 |
25 |
25.0 |
34 |
3.0 |
FR995-27 |
27 |
27.0 |
34 |
3.0 |
FR995-29 |
29 |
29.0 |
39 ± 3 mm |
3.0 |

Accessory
| Item number | Description |
|---|---|
| 7990SET | Freestyle™ obturator kit |
Related links
Similar products
-
 Avalus Ultra™ bioprosthesis
Avalus Ultra™ bioprosthesisThe Avalus Ultra™ bioprosthesis is a next-generation bovine pericardial valve for aortic valve replacement.
-
 Avalus™ bioprosthesis
Avalus™ bioprosthesisThe Avalus™ bioprosthesis is our first generation bovine pericardial valve.
-
 Hancock™ II bioprosthesis
Hancock™ II bioprosthesisThe HancockTM II bioprostheses are for patients who require replacement of their native or prosthetic aortic and/or mitral valves.
-
 Mosaic™ mitral bioprosthesis
Mosaic™ mitral bioprosthesisThe Mosaic™ mitral bioprosthesis is a next-generation native porcine valve for mitral valve replacement.
- Freestyle™ aortic root bioprosthesis 15-year clinical compendium, UC201606746EN.
- Klautz RJM, Rao, V, Reardon MJ, et al. Examining the typical hemodynamic performance of nearly 3000 modern surgical aortic bioprostheses. Eur J Cardiothorac Surg. 2024;65(5):ezae122. doi:10.1093/ejcts/ezae122.
- Perez de Arenaza D, Lees B, Flather M, et al. Randomized comparison of stentless versus stented valves for aortic stenosis: effects on left ventricular mass. Circulation. 2005;112(17):2696–2702. doi:10.1161/CIRCULATIONAHA.104.521161.
- Silberman S, Shaheen J, Merin O, et al. Exercise hemodynamics of aortic prostheses: comparison between stentless bioprostheses and mechanical valves. Ann Thorac Surg. 2001;72(4):1217–1221. doi:10.1016/s0003-4975(01)03064-8.
