What you need to know about hernia surgery? Consult your surgeon.

About hernia surgery
Hernia repair has been around for a long time. Treatments and techniques have improved over time and alternative options and materials have been developed. While not every technique is right for every hernia, they all have common goals — to provide the strongest repair and least chance of recurrence with minimal discomfort and quick recovery.

Before the surgery
A few days before surgery, the surgeon may order a pre-op exam consisting of blood tests, an EKG (electrocardiogram) and a chest X-ray to be sure the heart and lungs are in good condition. The surgeon will prescribe all necessary medications and any nutritional supplements required. The surgeon may also give a prescription for pain medication to take after surgery.

The day of surgery
When arriving at the hospital for surgery, consent forms will need to be signed as part of the admission process. Blood pressure will be taken and the patient will be given an IV (intravenous line). The patient's surgical area may need to be scrubbed and shaved to guard against infection.
The anesthesiologist will review the type of anesthesia required.
Medication may be given for relaxation before going to the operating room. In the operating room, the anesthesia will be administered and the procedure will be completed.
Consult your surgeon prior to having surgery.

Considerations
- Find a surgeon who specializes in hernia surgery and has experience with the latest techniques to make sure you have information on all of the options available.
- Make sure you understand the benefits and risks of your operation.
- Make sure to tell your surgeon about all medications and supplements you take; prescription, over-the-counter, and homeopathic.
The following is a list of questions to ask your surgeon:
- Which hernia repair procedures are you most comfortable with/do you perform the most?
- Which one do you recommend to fix my hernia and why?
- What risks are associated with this type of surgery?
- Do I have more than one option?
- What kind of anesthesia will I need?
- What is the recurrence rate with the recommended procedure?
- Do I need to stay in the hospital?
- Will my insurance cover the surgery?
- Will I need pain medication after surgery?
- When will I be able to return to work?
- When and how often will I need to see you for follow-up visits?

Understanding the risks1–4
Ensure that you discuss with a surgeon the benefits and risks of a surgical repair. An operation is the only way to repair a hernia. Typically, patients can return to normal activities and in most cases will not have further discomfort.
Possible risks include:
- Return of the hernia
- Infection
- Injury to the bladder, blood vessels, intestines, or nerves
- Difficulty passing urine
- Continued pain
- Swelling of the testes or groin area
Make sure to also discuss with your surgeon the risks of not having an operation. The hernia may cause pain and increase in size. If the intestines become strangulated or trapped in the hernia pouch it may cause sudden pain, vomiting, and an emergency operation will be required.
Types of hernia repair
Figure 1

Traditional open hernia repair1,2
An incision is made through the abdominal wall near the site of the hernia defect (Figure 1). The hernia is repaired with mesh or by suturing (sewing) the muscle closed. The incision can range from 5 cm to 10 cm in length depending on the size and location of the hernia, and also the surgeon’s technique. The incision is one of the major causes of pain after surgery.
Figure 2

Laparoscopic hernia repair1,2
This procedure is sometimes referred to as "keyhole surgery" (Figure 2). The hernia is repaired by mesh that is inserted through ports placed into small incisions in the abdomen, therefore eliminating the need for a large incision.
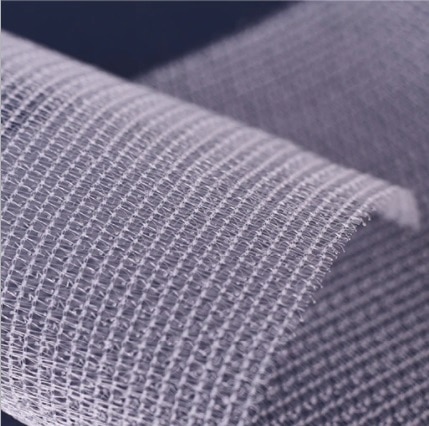
Non-tension
mesh repair
Non-tension means just that - instead of pulling the tissue around the hernia together, a piece of mesh is positioned to reinforce the area and fixed in place with sutures and/or tacks. The mesh is made of a flexible material that stays in the abdomen and encourages new tissue to grow into it. There are different kinds of mesh, including patches, three-dimensional, expanding, self-absorbing and self-gripping mesh that requires few to no sutures to keep it in place.
A mesh-based repair technique is recommended for patients with symptomatic inguinal hernias.1,2
Complications that may occur later following hernia repair surgery include persistent groin pain and post‐herniorrhaphy neuralgia, testicular complications, deep wound or mesh infection, recurrent hernia and mesh migration or erosion.

Traditional open repair
This method has been used historically and may be the only way to repair a very large hernia. The incision could potentially cause pain and recovery can take as long as five to six weeks. The incision also leaves a scar although it's usually very low on the abdomen.
In a traditional open hernia repair, the surgeon makes an incision near the hernia site and the hernia is reduced or pushed back into the abdomen. Most inguinal hernia repairs use mesh to close the defect.1,2
Complications that may occur later following hernia repair surgery include persistent groin pain and post‐herniorrhaphy neuralgia, testicular complications, deep wound or mesh infection, recurrent hernia and mesh migration or erosion.

Laparoscopic repair
Many inguinal hernias can be repaired using a laparoscopic procedure. Laparoscopic repair includes inserting special instruments through tiny incisions in the abdomen through which the surgeon is able to visualize and perform the procedure. Laparoscopic repair uses mesh and reinforcement. Provided that resources and expertise are available, laparoscopic techniques have fast recovery times, low chronic pain risk, and are cost effective.1,2
Laparoscopic procedures
- The surgeon makes three or four 6 mm –13 mm incisions in the abdomen. One is near the navel and the others are lower down.
- A laparoscope, a fiber optic tube with a tiny camera on the end, is inserted through one of the openings, allowing the surgeon to visualize the area on the monitor.
- The surgeon performs the procedure using surgical instruments inserted through the other openings while viewing it on the monitor. The mesh is positioned and fastened in place with sutures, tacks, or self gripping mesh.
- The instruments are removed. The holes are closed with a stitch or glue and covered with surgical dressings.
Laparoscopic hernia repair complications that may occur later following hernia repair surgery include seroma, urinary retention and infection, hematoma, visceral and vascular injury, nerve injury, testicular pain swelling, mesh and wound infection, bleeding, pulmonary and cardiovascular complications, and recurrence.
The clinical outcomes of each surgeon may vary due to different circumstances, experience and infrastructure. Please discuss with your local surgeon what treatment option is the most suitable for you.
Patients and caregivers: This information is designed to provide you with helpful educational information but is for information purposes only, is not medical advice, and should not be used as an alternative to speaking with your doctor. No representation is made that the information provided is current, complete, or accurate. Medtronic does not assume any responsibility for persons relying on the information provided. Be sure to discuss questions specific to your health and treatments with a healthcare professional. For more information, please speak to your healthcare professional.
Simons MP, et al. (2018) International guidelines for groin hernia management. Hernia. https://doi.org/10.1007/s10029-009-0529-7
Malangoni MA, Rosen, MJ. Hernias: In: CM Townsend, RD Beauchamp, et al. Sabiston textbook of Surgery, Philadelphia: Elsevier, 2012: Chapter 46.
Mesh versus non-Mesh for inguinal and femoral hernia repair. Cochrane Database Syst Rev. 2018; 2018(9): CD011517.
Risk factors for perioperative complications in inguinal hernia repair — a systematic review. Innov Surg Sci. 2017 Jun; 2(2): 47–52.